ADC Programs
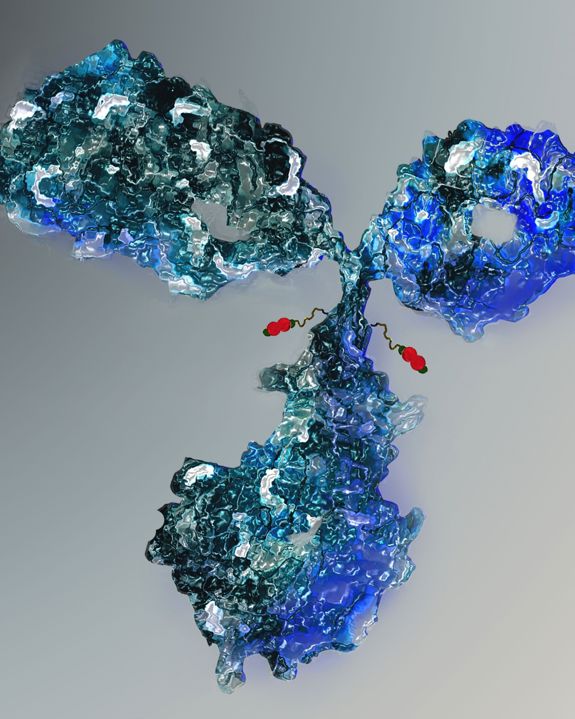
With two in-clinic programs and a clinically validated core platform, we are advancing a pipeline of differentiated ADCs for hard-to-treat cancers
We are focused on providing more effective treatments for patients who have few options, and our pipeline targets tumors including diffuse B-cell lymphomas, lung cancer, gynaecological tumors such as those of the ovary & cervix, pancreatic, gastric, triple-negative breast and colorectal cancer.
Our first wave ADC programs target antigens with proven premise in ADC formats and include novel DNA damaging payloads with tumor-activating pro-drug mechanisms.
ADC Programs
IKS03
CD19-directed ADC in Phase 1 clinical trials for B-cell cancers.
IKS03 has been designed to deliver high anti-cancer activity with good patient tolerability. The ADC benefits from tumor-selective activation and release of ultra-potent PBD payloads and preclinical studies have demonstrated class leading TI.
Best in class CD19-directed ADC for B cell cancers
The worldwide incidence of B-cell cancers is growing, especially in the older population.
There is high unmet need for patients with Diffuse Large B-cell Lymphoma (DLBCL), Mantle Cell Lymphoma and adult Acute Lymphoblastic Leukemia. DLBCL is a fast-growing lymphoma and is the most common type of non-Hodgkin lymphoma (NHL).
In the developed world, 5yr survival rates for B-cell NHL are around 70% and have increased over the last 25yrs, but almost 2 in 5 patients with diffuse cases (Stage IV and representing >1/3 of all newly diagnosed cases), die within 5yrs.
Despite active research and a strong pipeline, there are few effective therapeutic options for relapsed & refractory DLBCL. This form of lymphoma occurs predominantly in older people, (median age of diagnosis around 65ys) where approximately half of lymphoma patients cannot be cured, and even those who are cured must endure significant toxic chemotherapy effects. With increasing age, ALL patients have low clinical remission rates, high early mortality, high relapse rates and poor survival. Mantle Cell Lymphoma has no cure.
There is high demand for new, more effective and better tolerated options for relapsing & refractory patients. Better tolerated drugs are particularly relevant – most patients cannot tolerate intense, multi-drug chemotherapy or CAR-T.
CD19 is recognized as a relevant target for therapeutic development and the CD19-directed ADC Zynlonta was granted an accelerated approval for 3rd line use in patients with relapsed or refractory B-cell cancers based on a 48% response rate. Continued approval for this indication may be contingent upon verification and description of clinical benefit in a confirmatory trial(s).
Recently, the LOTIS-9 Phase 2 trial evaluating Zynlonta and Rituxan in unfit or frail patients with previously untreated DLBCL was terminated after the FDA placed a partial clinical hold on the trial. Several patients reported respiratory adverse events and seven patients died from extreme respiratory events. Alternative CD19-direwcted therapies with raised TI over Zynlonta represent a positive step in the treatment of this disease.
Recognising the value of targeting CD19 for B-cell cancers, Iksuda is developing an ADC with raised TI over Zynlonta, where lower doses drive more potent anti-cancer efficacy without being compromised by a low toxicity threshold. This is achieved through our use of tumor-selective release and activation of payload.
IKS014
HER2-directed ADC in clinical trials for HER2+ cancers.
IKS014 has been designed as a HER2-directed ADC with raised TI over in-clinic and on-market comparators, based on tumor-selective activation and release of the auristatin payload MMAF.
In Phase 1 clinical trials (as FS-1502 in China) in heavily pre-treated patients with advanced HER2+ breast cancer, its use is associated with an ORR equivalent to Enhertu (DESTINY-Breast01) and a favorable tolerability profile with notable absences of pulmonary toxicities, reduced neutropenia and thrombocytopenia and, unlike other MMAF-containing ADCs, no dose-limiting ocular toxicities.
HER2-directed ADC for HER2+ breast, lung, gastric & esophageal cancers
Amplification or overexpression of HER2 occurs in approximately 15% of all breast cancers & 10–30% of gastric/gastroesophageal and lung cancers and serves as a prognostic and predictive biomarker. HER2 overexpression also occurs in other forms of cancers including those of the stomach, ovary, uterine serous endometrial carcinoma, colon, bladder, uterine, cervix, head and neck, and oesophagus.
The introduction of Enhertu represents a major advance in the treatment of recurring, advanced and metastatic HER2-positive breast cancer but its toxicity profile is a cause for concern. Treatment-associated respiratory disorders (Interstitial Lung Disease/ pneumonitis) and blood & lymphatic disorders (neutropenia & anemia) are well-known and have resulted in patient deaths. Onset and grade of ILD/ pneumonitis is unpredictable and risk factors are not well understood.
The nausea, diarrhoea and severe fatigue associated with Enhertu represent major 'real world' issues according to physicians presenting at ASCO 2023. Around 2/3 of all patients treated with Enhertu experience nausea/ vomiting - a higher percentage seen with Kadcyla treatment.
There remains high need for additional HER2-directed therapies with more favorable toxicity profiles and, as Enhertu moves to earlier lines of treatment, more effective therapies are likely to replace Kadcyla after Enhertu therapy.
New HER2-directed therapies which match the efficacy of Enhertu but with more favorable toxicity profiles represent a step forward in the treatment of HER2+ cancers.
IKS014 has been designed to be a class-leading HER2-directed ADC for all HER2+ solid tumors, with raised TI over Enhertu and other in-clinic & on-market comparators.

IKS04
Ultra-low DAR, CA242-directed ADC in preclinical development for GI tumors.
IKS04 is the only CA242 (CanAG)-directed ADC in development and has been designed to deliver high anti-cancer efficacy and manageable tolerability in some of the hardest to treat solid tumors.
IKS04 represents a new 'ultra-low DAR' ADC approach to overcome issues often seen with targeted drug delivery to solid tumors. Targeting an antigen with high tumor selectivity and high expression abundance, our approach drives effective tumor penetration and tumor-specific delivery of ultra-potent payloads, enabling a drug with increased efficacy and class-leading TI.
CA242-directed ADC for GI tumors
CanAg, a novel glycoform of MUC1, is a ‘tumor antigen’; an antigenic substance produced in tumor cells and that trigger an immune response in the host. The MUC1 protein serves a protective function by binding to pathogens and also functions in a cell signaling capacity. Overexpression, aberrant intracellular localization, and changes in glycosylation of this protein have been associated with carcinomas.
Since it is a tumor antigen, CanAg represents a favorable target for immune-oncology therapeutic approaches, and may be especially relevant to ADCs, combining the immunity-reversing mechanism of a CanAg antibody with potent cell-killing payloads.
Successful CanAg-targeted therapeutics should impact some of the most challenging tumors. CanAg has been clinically validated as a target in various solid tumors, but IKS04 is the only active program today.
CanAg is expressed in almost all pancreatic, biliary tract & colorectal cancers, 55% of gastric cancers, 45% of uterine (endometrial) cancers and 40% of NSCLC & bladder cancers.
Over 1/3 of patients who undergo surgery with curative intent develop a recurrence of pancreatic cancer, despite adjuvant chemotherapy.
Colorectal cancer ranks 3rd in terms of incidence of all cancers but 2nd in terms of mortality. Most patients present with advanced disease, with a 5yr survival rate of only 14%. 40% of patients recur within 2-3 years of treatment.
Approximately 50% of patients with bladder cancer develop recurrence after cystectomy.
Stomach cancer is the 5th most common cancer in the world. Unfortunately, due to the lack of effective screening, many patients are diagnosed with advanced (Stage 3 or Stage 4) disease. As a global average, 5yr survival for all stages of stomach cancer is around 20%, with only 30-40% surviving a year. For patients with Stage 2 disease the 5yr survival rate is around 30%, whilst this falls to 25% for Stage 3 and virtually zero for Stage 4.
Lung cancer has been the most common cancer in the world for several decades, accounting for 1 in 5 of all cancer deaths: worldwide, 3 people die from lung cancer every minute, more per year than breast, colorectal and prostate combined. Approximately 40% of lung cancer patients are diagnosed with metastatic disease where 5yr survival is <5%.
Since effective therapy options for GI tumors are suboptimal or unavailable, IKS04 has been designed to deliver ADC power with a suitable TI. Iksuda has selected target antigen with high tumor selectivity and high expression abundance. We then deliver an ultra-low DAR ADC to drive good tumor penetration, and deliver an ultra potent DNA cross-linker payload through tumor-selective activation & release.
IKS012
Class leading FOLR1-directed ADC in preclinical development for ovarian cancer.
IKS012 has been designed to extend provide a new therapeutic with raised TI over in-clinic and on-market FOLR1-targeting ADCs. It benefits from tumor-selective activation and release of MMAE. In preclinical studies, it demonstrates a class-leading profile, with high anti-cancer activity in FOLR1-high xenograft models and a substantially higher HNSTD in non-human primates than its competitors.
FOLR1-directed ADC for ovarian, lung and triple-negative breast cancers
Folate receptor alpha (FOLR1) is an attractive target for cancer drugs against solid tumors of high unmet need and poor prognosis. FOLR1 is frequently overexpressed in several human malignancies including cancers of the ovary, lung and breast.
Elevated FOLR1 expression is associated with lower DFS and poor OS in patients with ovarian cancer of serous origin. Both common subtypes of NSCLC express high levels of FOLR1; high expression is observed in lung adenocarcinomas – the most common type of lung cancer diagnosed in patients who have never smoked.
FRα is overexpressed in hard-to-treat breast cancers, including ER/PR-negative & triple negative (TNBC) and this is significantly associated with high histologic grade & advanced stage and high proliferative activity.
Ovarian cancer: FOLR1 is overexpressed in 80% of epithelial ovarian cancers (EOCs), with medium-high expression in 60% of cases. Ovarian cancer (OC) is the 7th most common cancer among women in the world and is the 5th most common cause of cancer death in women. If diagnosed at localized stage, 5yr survival rate is high but only 15-20% (according to country) are diagnosed at this stage. The late-diagnosis 5yr survival rate is around 30% - and only 17% for Stage 4. Relapsed Ovarian Cancer (OC) carries a poor prognosis. Effective and tolerable agents used to treat this disease therefore represent a significant unmet medical need.
Lung cancer: Lung cancer has been the most common cancer in the world for several decades, accounting for 1 in 5 of all cancer deaths: worldwide, 3 people die from lung cancer every minute, more per year than breast, colorectal and prostate combined. NSCLC accounts for around 80% of lung cancer cases. FOLR1 is overexpressed in the majority of NSCLC, particularly in lung adenocarcinomas.
Breast cancer: High FOLR1 tissue expression in 80% of TNBC patients and >70% of ER/PR-negative tumors, leading to poorer DFS. TNBC represents 10-20% of all breast carcinomas; it is an aggressive disease which accounts for a disproportionate number of metastatic cases and deaths.
Iksuda is developing a class leading FOLR1 ADC with higher anti-cancer efficacy in FOLR1-high expressing tumors. Our premise is to enhance TI over on-market & in-clinic comparators, driving increased efficacy over Elahere (mirvetuximab soravtansine) and a markedly improved safety profile over both Elahere and Farletuzumab ecteribulin.
Pipeline prioritization strategy
When designing our ADCs, Iksuda evaluates the best technology available for each ADC component, testing and honing the construct to achieve an optimal profile. If the lead candidate achieves or exceeds our benchmark TI, established to ensure clinical meaningful differentiation vs in-clinic or on-market comparators, we progress through IND enabling studies.